Is the NHS using your money wisely?
Stories about people who have been denied life-saving drugs regularly make the headlines. Many of us have been personally affected by a treatment not being available on the NHS.
So how does the NHS decide which drugs or treatments to fund, and which not to?
Trust Me lined up two experts with differing views to discuss this question.
First, Professor Karl Claxton. He is a health economist who believes that NICE, the body that advises the NHS, is approving too much spending on new drugs.
He believes there is a skew towards new, costly drugs at the expense of other effective NHS treatments that should be made available to more patients.
He feels there is a huge discrepancy between what NICE is approving and what the NHS can actually afford.
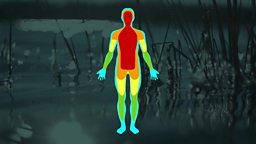
Most NHS money is spent on patients during the final stages of their life, and Prof Claxton believes there is no evidence to suggest that society wishes this to be the case.
In his opinion, the resources devoted to extending the end of life, sometimes of very sick people, could be better spent on cheaper treatments that are proven to be highly effective, such as interventions in common mental health problems, or hip replacements. These treatments can significantly prolong life and increase the quality of life for many.
He acknowledges that if a cancer patient is offered an expensive new drug then they will of course want access, but that the solution to this problem is to review drug pricing, so that it reflects how much the NHS can afford to pay for the scale of the benefits that a drug offers.
Next, Dr Jane Adam, who chairs one of NICE’s independent committees that make recommendations to the NHS about funding new medications and treatments.
She believes that the spending emphasis on end of life can be defended. If someone is going to die of their disease within two years, and that a new treatment will give them at least 3 months extra life, then it is legitimate to give that treatment a higher value than it would at other times in life. This weighting is made on the basis that when you are dying, those extra few months can be particularly precious, but that this is a decision that we must make as a society.
She defends NICE’s mechanism for approving drugs. In the current system, if a drug is very effective and brings a huge amount of benefit to patients, then the NHS will pay more for it. But if it is of relatively limited benefit, then it has to still be good value, which means it must be cheaper.
She feels the importance of a rigorous approval process is essential given that the NHS budget is limited and under strain.
Anyone can comment on NICE’s decisions.